Hydroxychloroquine prophylaxis for COVID-19 contacts in India
More than a billion Indians currently stand at the precipice of a massive increase in cases of coronavirus disease 2019 (COVID-19).
India had shown a staggered course of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission, with 1397 cases diagnosed between Jan 31, and April 1, 2020.
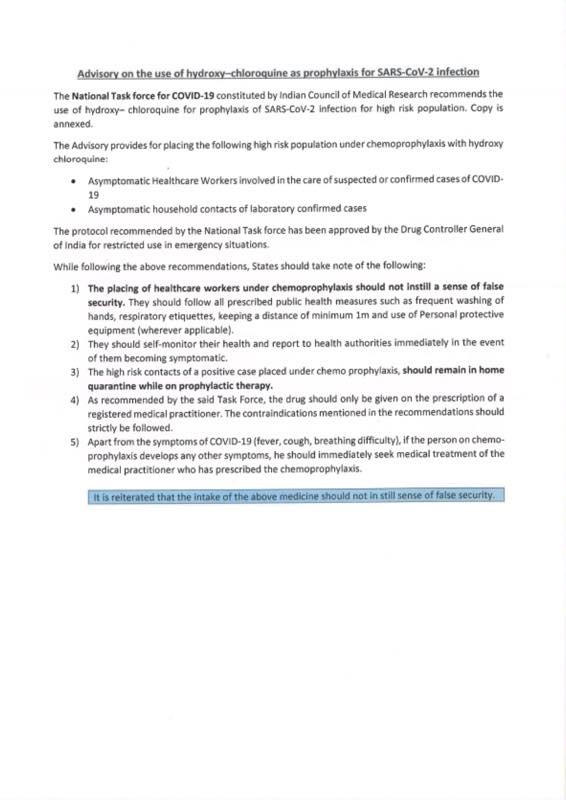
However, there has been a recent surge in cases, with numbers rising to 5194 as of April 8. The Indian Council of Medical Research, under the Ministry of Health and Family Welfare, has recommended chemoprophylaxis with hydroxychloroquine (400 mg twice on day 1, then 400 mg once a week thereafter) for asymptomatic health-care workers treating patients with suspected or confirmed COVID-19, and for asymptomatic household contacts of confirmed cases.
The document states “its use in prophylaxis is derived from available evidence of benefit as treatment and supported by preclinical data”. Although some in-vitro evidence supports the antiviral activity of hydroxychloroquine and its precursor chloroquine, there is no peer-reviewed publication that evaluates either drug for exposure prophylaxis of SARS-CoV-2 infection.
Even for treatment of diagnosed cases, only one small study reported faster nasopharyngeal viral clearance, with no data for clinical improvement.
This evidence, or the lack thereof, hardly justifies state-endorsed, widespread use of hydroxychloroquine for prophylaxis.
We are deeply concerned that in this environment of global panic, an endorsement by the highest scientific body of India (and also by the President of the USA) will create an overly optimistic perception of the effectiveness of hydroxychloroquine among the public.
Markets in the USA are already reporting a short supply of both hydroxychloroquine and chloroquine.
The situation in India is no different, probably indicating widespread self-medication.The shortage of chloroquine, an inexpensive antimalarial in low-income malaria-endemic countries like India, could lead to preventable morbidity and mortality. Moreover, mathematical models estimate a worst-case scenario of 10 million cases of COVID-19 in New Delhi, India, alone in the coming weeks.
In these chaotic times, no health-care system can screen such a large number of healthy contacts for concomitant QTc prolonging medicines, long QT syndromes, or glucose-6-phosphate dehydrogenase deficiency.
Even a 0·1% proportion of serious complications would amount to more than 10 000 severe adverse events in New Delhi alone, a number an already overwhelmed health-care system would not be able to cope with. The drug is untested, the benefits unknown, and the risks not negligible, especially at this scale of use. Moreover, the safety of these immunomodulators in people at risk of a severe viral illness has never been evaluated.An ongoing pandemic justifies leeway in generation and interpretation of evidence in the interest of public health.
However, all scientific reasoning cannot be abandoned citing desperate times. A blanket recommendation for chemoprophylaxis in the absence of credible evidence might be contentious to say the least.
If hydroxychloroquine is to be used, a clear informed choice needs to be offered to every contact, explaining the scarcity of evidence for its efficacy and its potential risks.
Additionally, all outcome events should be recorded. If this is not done, the risk–benefit assessment would be skewed, adverse events accepted as collateral damage, and a drug accepted provisionally in a time of crisis could become commonplace as standard of care for a long time to come.


See the full original article here: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30313-3/fulltext#coronavirus-linkback-header
See approval document from the Indian Council of Medical Research, under the Ministry of Health and Family Welfare: https://www.mohfw.gov.in/pdf/AdvisoryontheuseofHydroxychloroquinasprophylaxisforSARSCoV2infection.pdf