Source: medRxiv, full study here
ABSTRACT:
Objectives:
A decrease in blood cell counts, especially lymphocytes and eosinophils, has been described in patients with severe SARS-CoV-2 (COVID-19), but there is no knowledge of the potential role of their recovery in these patients’ prognosis. This article aims to analyse the effect of blood cell depletion and blood cell recovery on mortality due to COVID-19.
Design:
This work is a multicentre, retrospective, cohort study of 9,644 hospitalised patients with confirmed COVID-19 from the Spanish Society of Internal Medicine’s SEMI-COVID-19 Registry.
Setting:
This study examined patients hospitalised in 147 hospitals throughout Spain. Participants: This work analysed 9,644 patients (57.12% male) out of a cohort of 12,826 patients ≥18 years of age hospitalised with COVID-19 in Spain included in the SEMI-COVID-19 Registry as of 29 May 2020. Main outcome measures: The main outcome measure of this work is the effect of blood cell depletion and blood cell recovery on mortality due to COVID-19. Univariate analysis was performed to determine possible predictors of death and then multivariate analysis was carried out to control for potential confounders.
Results:
An increase in the eosinophil count on the seventh day of hospitalisation was associated with a better prognosis, including lower mortality rates (5.2% vs 22.6% in non-recoverers, OR 0.234 [95% CI, 0.154 to 0.354]) and lower complication rates, especially regarding to development of acute respiratory distress syndrome (8% vs 20.1%, p=0.000) and ICU admission (5.4% vs 10.8%, p=0.000). Lymphocyte recovery was found to have no effect on prognosis. Treatment with inhaled or systemic glucocorticoids was not found to be a confounding factor.
Conclusion:
Eosinophil recovery in patients with COVID-19 is a reliable marker of a good prognosis that is independent of prior treatment. This finding could be used to guide discharge decisions.
KEYWORDS:
2019-nCoV;
SARS-CoV-2;
coronavirus;
COVID-19;
eosinophil;
prognosis
INTRODUCTION:
In December 2019, a pneumonia of unknown origin was described in the city of Wuhan, the capital of Hubei province in China, caused by a novel coronavirus that was later named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) (1). The infection was named COVID-19 (COronaVIrus Disease 2019) in February (2) and later labelled a pandemic (3). As a result of its global spread, overwhelming almost every healthcare system, COVID-19 has become the greatest health emergency of this century. As of 23 June, nearly 9 million COVID-19 cases had been confirmed, and 469,587 patients had died. Initially, Europe was one of the most affected continents, with more than 2.562 million cases;
Spain accounted for 246,504 of those cases (4). Great effort has been made in describing the clinical and epidemiological features of COVID-19 (5–7), yet less is known about prognostic factors (8–10). Older male adults and those with diabetes, hypertension, obesity, cardiovascular disease, or chronic respiratory disease are at greater risk of developing severe COVID-19. Some prognostic factors upon admission are lymphopenia and high levels of D-dimer (DD), lactate dehydrogenase (LDH), and C-reactive protein (CRP) (11).
Some studies have reported low total eosinophil counts in COVID-19 inpatients and persistently low eosinophil counts in more severe cases (12–15). A correlation between eosinophil recovery and radiographic and virologic recovery (13) as well as a worse prognosis when eosinophil levels do not recover have been suggested (14). A meta-analysis of those reports, however, found no effect of eosinophil counts upon admission or eosinophil recovery during the course of COVID-19 (15).
The Spanish Society of Internal Medicine (SEMI, for its initials in Spanish) has launched the SEMICOVID-19 Network, a nationwide, collaborative effort to compile information on patients hospitalised with COVID-19. In a preliminary study (not yet published) of potential prognostic factors, recovery from both lymphopenia and eosinopenia correlated with a lower risk of death on a multivariate analysis. We decided to conduct a specific analysis to demonstrate whether eosinopenia or eosinophil recovery could be a prognostic factor against death due to COVID-19.
HYPOTHESIS AND OBJECTIVES:
According to our preliminary data, we hypothesised that recovery from eosinopenia could serve as an independent predictor of a favourable outcome in patients with COVID-19. The primary aim of the study was to evaluate whether eosinophil recovery was a predictive factor of favourable progress during hospitalisation in COVID-19 patients. The secondary aims were a) to explore the relationship between recovery from eosinopenia and the development of acute respiratory distress syndrome (ARDS), b) to evaluate the possible confounding effects of the use of corticosteroids in these patients, and c) to evaluate the possible confounding effects of prior comorbidities that affect eosinophil counts.
METHODS:
Registry Design and Data Collection. The SEMI-COVID-19 Registry is an ongoing, nationwide, retrospective cohort that includes consecutive patients with a confirmed COVID-19 infection who have been hospitalised and discharged from Spanish hospitals. The registry’s characteristics have been thoroughly described in other works (16). Inclusion criteria for the registry are age ≥18 years and first hospital discharge with a confirmed diagnosis of COVID-19.
Exclusion criteria are subsequent admissions of the same patient and denial or withdrawal of informed consent. From 24 March to 29 May 2020, a total of 12,826 discharged patients were included in the registry. Patients are treated at their attending physician’s discretion, according to local protocols and clinical judgement. Patients included in open-label clinical trials are eligible for inclusion in the registry provided that all information about treatment is available. Data from medical records are collected retrospectively at discharge by clinical investigators all over the country, using a standardised online data capture system (DCS) described elsewhere (1.6).
Data collected includes many variables, collected and defined in more detail in The SEMI-COVID-19 Registry (16) The Spanish Society of Internal Medicine is the sponsor of this registry. The researchers who coordinate the study at each hospital are SEMI members and have been asked to participate in the study on a voluntary basis; they do not receive any remuneration for their participation. Data confidentiality and patient anonymity were maintained at all times, in accordance with Spanish regulations on observational studies. This study was carried out in accordance with the Declaration of Helsinki and was approved by the Institutional Research Ethics Committees of each participating hospital.
Study Design A retrospective cohort study was designed in order to control for potential confounding variables. Patients included in the SEMI-COVID-19 Registry as of 31 May 2020 were selected for inclusion in this study if they had: a) all epidemiological data recorded, b) data on lymphocyte and eosinophil counts upon admission and on the secondary analysis at seven days after admission , and c) onset of symptoms prior to admission. This last criterion was necessary given that the registry included nosocomial infections and, since laboratory analyses were performed upon admission and on the seventh day of hospitalisation, this ensured that the values did not correlate to clinical progress in nosocomial infections.
A descriptive analysis of the cohort and a multivariate analysis for prognostic factors were performed. Variables that have previously been demonstrated in a literature search to be correlated with eosinophil count (such as asthma or chronic corticoid use) or with COVID-19 severity or progress were considered for multivariate analysis. Variables selected for analysis included demographical variables (age, sex, race, obesity, hypertension, diabetes, alcohol abuse, tobacco use, chronic kidney disease, chronic respiratory diseases, comorbidity burden, degree of dependency, and use of inhaled or systemic corticosteroids); clinical variables (signs and symptoms upon admission, laboratory results and radiographic findings upon admission); treatment received prior to the second laboratory analysis; results of the second laboratory analysis; and clinical outcomes (specifically, pneumonia, ARDS, acute kidney injury, sepsis, ICU admission, and death).
Eosinopenia was defined as a total eosinophil count <150 x 106 /L upon admission. Eosinophil recovery was defined as an elevation greater than 80 x 106 /L on the second analysis performed on the seventh day of hospitalisation. Lymphopenia was classified into four categories: <800, 800-999, 1000-1199, and ≥1200. Lymphocyte recovery was defined as an elevation greater than 200 x 106 /L on the second analysis. QuickSOFA index (qSOFA) was calculated from the physical findings upon admission. All other quantitative variables were categorised as normal or abnormal (according to reference levels) upon admission. Evolution of significant values during the hospital stay were categorised as absolute elevation (for D-dimer or glycaemia) or relative elevation (for LDH, AST, ALT, and creatinine).
The STROBE Statement guidelines were followed in the conduct and reporting of the study. Statistical Analysis In the descriptive analysis, we summarised the epidemiological data, demographics and comorbidities, signs and symptoms upon admission, laboratory upon admission and on the seventh day of hospitalisation, chest radiography findings, treatment received , and clinical outcomes.
We performed an initial univariate analysis to determine any differences between eosinophil-recoverers and non-recoverers. We then performed a second univariate analysis to determine factors that correlated with death. Continuous variables are expressed as means and standard deviation (SD); categorical variables are expressed as absolute values and percentages.
We conducted the analysis by means of the Student’s t-test for quantitative variables and the chi-square test or Fisher’s exact test to compare differences between groups. A univariate analysis was performed to explore possible risk factors for death using binomial logistic regression. Variables associated either with eosinophil recovery (potential confounding factors) or with death were included in a backward stepwise multivariate logistic regression model.
Survival analysis was deemed unnecessary, as each patient was discharged and the date of discharge or death was recorded in the registry, as per its design, and time until death or discharge was not considered relevant. Quantitative variables were categorised as normal or abnormal upon admission and significantly elevated or not significantly elevated at seven days of hospitalisation.
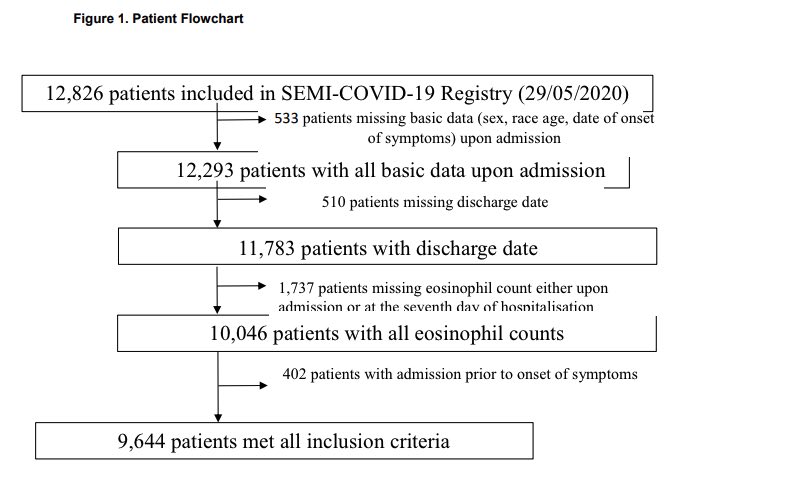
A secondary multivariate analysis was conducted with the composite endpoint of in-hospital death, ICU admission, or onset of moderate-to-severe ARDS. We used SPSS (v. 25, IBM Corporation, 2017) for all analyses. RESULTS: Sample characteristics The SEMI-COVID-19 Registry included 12,826 patients as of 29 May 2020. Of them, 533 did not have all demographic and epidemiological data recorded (sex, age, race, and date of onset of symptoms) and thus were excluded. Another 510 patients were excluded because their discharge date was not recorded.
Of the 11,783 discharged patients with all epidemiological data available, 282 were excluded because they did not have eosinophil counts upon admission and a further 1,455 were excluded for not having eosinophil counts on the seventh day of hospitalisation. Finally, 402 patients had been admitted prior to onset of symptoms and were thus also excluded. A total of 9,644 patients fulfilled all inclusion criteria for this study. Of these, 3,335 patients (34.6%) had eosinophil recovery whereas 6,309 patients (65.4%) did not.
Figure 1 shows the flowchart for patient inclusion. Demographic and clinical features of the study cohort are described in Table 1. There were differences upon admission between patients who showed eosinophil recovery and those who did not. Some important features, such as sex, obesity, or asthma, did not differ. Non-recoverers had a higher overall age and higher rates of hypertension, diabetes, chronic kidney disease (CKD), and chronic obstructive pulmonary disease (COPD).
Recoverers, on the other hand, had higher comorbidity burdens and a greater degree of dependency. Clinical presentation also differed between recoverers and non-recoverers. Recoverers had a longer duration of symptoms prior to admission, higher rates of cough and arthromyalgia, and lower rates of dyspnoea. Confusion and tachypnoea were more frequent in non-recoverers. There were no differences in temperature, heart rate, or arterial systolic tension, but oxygen saturation were lower in non-recoverers.
A higher proportion of non-recoverers also had a qSOFA index ≥2. Non-recoverers had worse laboratory analysis profiles upon admission, with higher glucose, creatinine, D-dimer, and LDH levels. Lymphocyte counts were not significantly different, but eosinophil counts were lower among recoverers. Pulmonary infiltrates on radiological tests were more frequent in eosinophil recoverers.
Treatments and outcomes are summarised in Table 2. Eosinophil-recoverers were more frequently treated with hydroxychloroquine and less frequently treated with systemic or inhaled glucocorticoids. There were no differences between recoverers and non-recoverers regarding treatment with lopinavir-ritonavir, azithromycin, or low-molecular-weight heparin. All outcomes were better among eosinophil-recoverers, with lesser rates of pneumonia, ARDS, acute kidney injury, sepsis, ICU admission, and death.
Notably, 94.8% of eosinophil-recoverers were discharged alive (vs 77.4% in non-recoverers, p<0.001), 91.3% were discharged without requiring ICU admission (vs 71.1% in non-recoverers, p<0.001), and 85.8% were discharged with neither ICU admission nor onset of ARDS during hospitalisation (vs 65.5% in non-recoverers, p<0.001). Outcomes Variables that correlated with either mortality or eosinophil recovery upon univariate analysis (Table 3), as well as potential confounding factors, were introduced into a multivariate analysis using mortality as the dependent variable. Several models were checked for sensitivity analysis, changing cut-off points for categorisation.
The final model is summarised in Table 4 and shows that eosinophil recovery was independently associated with lower mortality, with an OR of 0.234 (95% CI, 0.154 to 0.354). Initial eosinopenia was not found to be significant in the model. A lymphocyte count lower than 800 x 106 /L upon admission was predictive of death, but neither further categorisation of lymphocyte value ranges nor lymphocyte recovery was. Corticosteroid treatment was not found to correlate with death in our model whereas both
Notably, both elevated ALT upon admission and at seven days of hospitalisation correlated with a lower mortality rate. More studies are needed to clarify this finding. A secondary multivariate analysis was performed for the secondary composite endpoint of in-hospital death, ICU admission, or onset of ARDS during hospitalisation (Table 5), After controlling for other variables, eosinophil recovery was found to correlate with a lesser chance of worse progress (OR 0.474; 95% CI, 0.383-0.586).
DISCUSSION
Our study shows that eosinophil recovery has a positive prognostic impact in COVID-19 that is independent of previous lymphocyte or eosinophil levels and previous use of systemic or inhaled corticosteroids. To the best of our knowledge, this work is the first instance that this prognostic factor has been identified and described. Abnormal laboratory values in patients with COVID-19, in particular low levels of lymphocytes, have been described in several studies, but less emphasis has been placed on low levels of eosinophils.
Lymphocyte depletion has been shown to have diagnostic value, along with prognostic value shown in various studies, albeit inconsistently. Eosinophil depletion has been anecdotally described, mostly in small series (12,13). The recovery of lymphocytes and eosinophils has been studied to a lesser degree than the implications of their initial values (14). A previous meta-analysis of 294 subjects (15) showed that eosinophil levels made no difference in the progress and mortality of patients with COVID-19.
In our cohort, which comprises 9,644 patients, a profound degree of eosinopenia was found upon diagnosis of COVID-19, with a higher mortality rate observed in eosinopenic patients than in non-eosinopenic patients (16.7% vs 13.2%, p 0.04). Furthermore, eosinophil recovery was associated with higher survival rates, as was found by Sun et al . (14).
However, these findings could have been due to a number of confounding factors, the most obvious being that comorbidities or immunosuppressive drugs (used predominantly in more severe cases) could be responsible for the prolonged eosinopenia and thus eosinophil recovery would be a marker of other previous prognostic factors. Another explanation could be that eosinophil levels and eosinophil recovery are parallel to lymphocyte levels, representing the same degree of immune response to SARS-CoV-2.
The most obvious potential confounding factor is prior use of glucocorticoids, which have been widely described as a cause of eosinopenia by means of medullary retention. For this reason, we designed our study to control for the use of systemic or inhaled glucocorticoids both before and during hospitalisation as a potential confounding factor in sustained eosinopenia and COVID-19 progress.
The multivariate analysis showed no effects of chronic or acute use of corticosteroids, asthma, or other diseases that affect eosinophil levels on the predictive capacity of plasmatic eosinophils. In our analysis, asthma or pulmonary infiltrates on radiological tests did not significantly correlate with mortality and were eliminated from the model. The elevation of eosinophils was found to be associated with a better prognosis and lower mortality rate, with an OR of 0.234 (95% CI, 0.154 to 0.354), independently of previous use of glucocorticoids.
Our results are in contrast to the conclusions of the meta-analysis by Lippi et al. (15) and corroborate the work by Sun et al. (14). All these findings emphasise the yet-unexplored role of eosinophils as an immunomodulatory factor in COVID-19. Our results could be explained by either distinct initial inflammatory responses to SARS-CoV-2, with an initial predisposition towards a Th2 response, or by different inflammatory evolutions, with an immune recovery with modification from an initial Th1 inflammatory response to a Th2 response (17), or indeed both of them simultaneously.
Eosinophil recovery could be a marker of a different inflammatory pathway associated with mortality. Several studies have demonstrated the key role of eosinophils in the initiation and maintenance of inflammation through stimulation of a Th2 inflammatory response as well as their direct association with inflammatory diseases such as asthma (18–20). Curiously, asthma, which was initially suspected to be a risk factor in COVID-19, has been consistently shown to have a protective role in various cohorts (4,9,12), except for severe asthma, which may be neutrophilic asthma not mediated by a Th2 response.
If an underlying Th2 response is involved in eosinophil recovery, it would be expected that we would find a higher proportion of asthmatic patients amongst eosinophil-recoverers and higher levels of eosinophils upon admission. However, in our series, eosinopenia was more severe in eosinophil-recoverers and thus does not suggest a Th2 response prior to admission. On the other hand, patients with obesity and type 2 diabetes mellitus are known to have a higher Th1 inflammatory response (21,22) and to have a worse COVID-19 prognosis (8,10,23).
Both greater eosinopenia and lower recovery of eosinophil counts could simply be markers of these previous comorbidities, as both diabetes and obesity were more prevalent among non-recoverers. Our univariate analysis confirmed higher mortality rates amongst patients with obesity and diabetes, but this effect disappeared in the multivariate analysis. Therefore, it could well be the other way round: instead of eosinophil recovery being a surrogate for lower diabetes rates, the latter could be a deleterious factor because it implies an intrinsic Th1 response, leading to a worse prognosis for COVID-19. Another possible immunological explanation for the role of eosinophils could be that, regardless of the initial response to SARS-CoV-2 infection, eosinophil recovery represents a marker of immune recovery.
This could also be due to a non-specific pathway or to Th2 switching. Were it due to non-specific recovery, it would merely be a marker of good progress with no special immunological significance and should be paralleled or followed by lymphocyte recovery. Our study shows that lymphocyte recovery at the seventh day of hospitalisation is not an independent marker of a good prognosis whereas Sun et al. (14) found an elevation in lymphocyte counts in less severe cases, but starting later than eosinophil recovery.
Our database only includes two laboratory analyses (upon admission and on the seventh day), so it is not possible for us to ascertain whether a later lymphocyte recovery exists or if it has prognostic implications or not. Regardless, a marker of a good prognosis after the seventh day of hospitalisation is probably less useful than an earlier predictor would be.
On the other hand, eosinophil recovery could be a marker of Th2 switching, thus possibly indicating a different inflammatory response to SARS-CoV-2 and leading to less susceptibility to ARDS. This is a highly interesting explanation that should be studied further, as it could well lead to new therapeutic strategies for COVID-19. Different immunological profiles have been described in other inflammatory diseases of both autoimmune and infectious origin.
The ones most commonly described are the Th1 pathways (involving the so-called Th1 cytokines of IL-12, IFN, and TNF-α, leading to activation of CD8+ T cells and classically activated macrophages), the Th2 pathways (mediated by IL-4, IL-5, and IL-13, leading to activation of eosinophils, alternatively activated macrophages, and B-lymphocytes), and the Th17 pathways (mediated by IL-1, IL-6, and the inflammasome, leading to IL-17 and IL-22). In COVID-19, cytokine elevation has been described as a marker of worse progress (higher ARDS and death rates), with involvement serum levels of both IL-1 and IL-6.
These patients probably develop a Th1-Th17 response to the infection. A depletion of Treg lymphocytes, which are crucial for the negative regulation of proliferation and inflammation, has been described in COVID-19 patients, especially in more severe cases (24). There is no knowledge of the mechanism of lung inflammation, as live biopsies have not been described to date.
Autopsies after ICU death have shown low-grade inflammation and high rates of local microthrombosis (25), but this may be the advanced, terminal stage of a previous inflammatory injury. Different inflammatory pathways could explain the different progress observed amongst COVID-19 patients. It may not be a question of whether an inflammatory response is provoked, but rather which inflammatory response is provoked.
Lessening cytokine dysregulation with immunosuppressants has already been attempted. Perhaps efforts towards inducing a Th2 response could improve patient prognosis but, to our knowledge, there is no pharmacological pathway to do so. In our study, we explored other changes in the laboratory findings over the course of a patient’s disease.
Our multivariate model showed the significance of ALT, LDH, creatinine, and D-dimer elevation. Another finding in our study is the protective effect of both hydroxychloroquine and azithromycin observed in our model.
These findings should be interpreted cautiously, as our study was not designed to control for confounding factors of renal or hepatic function. Finally, we also explored the composite endpoint of in-hospital death, ICU admission, or onset of ARDS during patients’ hospital stay. Eosinophil recovery also correlated favourably with this outcome, with an OR of 0.474 (95% CI, 0.383 to 0.586), meaning that not only was death less frequent among eosinophil-recoverers, but a milder course could be predicted.
This is highly important, as eosinophil recovery is a marker of a good prognosis and could be used to guide decisions regarding discharge in otherwise stable patients. In the context of a pandemic, this could help alleviate the strain on healthcare systems by identifying potential candidates for early discharge. Among the strengths of the SEMI-COVID-19 Registry and its consequent studies are its multicentre, nationwide design along with the large number of patients included, which provides strong statistical power for confirming hypotheses.
However, for the same reason, all the studies based on the SEMI-COVID-19 Registry have common limitations. As only inpatients were included, it is not possible to extrapolate our results to outpatients. Information bias could be introduced by either the large number of researchers involved or variability in the availability of data from each hospital.
Finally, selection bias could be introduced given the voluntary participation of each centre. Our study was designed to control for possible confounding factors for abnormal eosinophil values, but some of them could not be controlled for due to the nature of the data available in the registry. Transfusion of blood products was not recorded and thus this information is not available for study.
The influence of the stress response and hormonal treatment were also not recorded, but should be taken into account when assessing haematological parameters. Bacterial coinfection during or superinfection after contracting SARS-CoV-2 could have led to different immune responses.
Neither thorough cytokine profiles nor lymphocyte subset panels were obtained, as this registry reflects usual clinical practice and not basic research, so inflammatory pathways were not studied. Further research is needed to overcome these limitations.
In conclusion, eosinophil recovery at the seventh day of hospitalisation is a predictor of a good prognosis in COVID-19 and warrants further research.
CONCLUSIONS:
Eosinophil recovery, independently of treatments administered and the patients’ underlying condition, is a marker of good prognosis and could help in making decisions about safe discharge. – More studies are needed to assess whether eosinophil recovery is a marker of general immune recovery or of a different immunological response profile to the infection.
Figures






Related: