Source: PGibertie
THE INDIAN MODEL PROVES THAT WE HAVE EVERYTHING FALSE: he defeated the virus with hydroxychloroquine and ivermectin, uses a traditional vaccine, exports experimental vaccines for these idiots of Westerners …
India is the first country in the world for the production of drug molecule, but it is also a developing country. Populated by 1.4 billion inhabitants, it still has 90 million over 60 years also exposed to covid. It is the second country in the world for no number of cases. India followed the Raoult and Borody protocol to the letter …
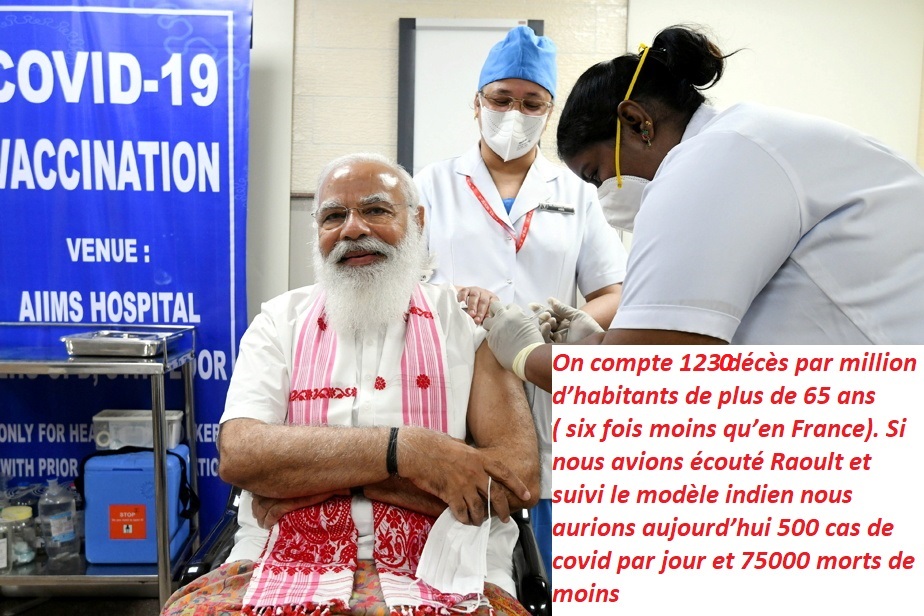
The reproduction rate of the virus continues to decline and the country which has known at least 11 million declared cases has reached the threshold of collective immunity. There are 1,230 deaths per million inhabitants over 65 (six times less than in France). If we had listened to Raoult and followed the Indian model, today we would have 500 cases of covid per day and 75,000 fewer deaths …
Today India’s vaccine choices are surprising, the country produces astrazenneca vaccine for export, and has made an Indian version of it for export as well. Geopolitical weapon the country gives these vaccines to other countries.
But for the Prime Minister and the people India is making a traditional vaccine without messenger RNA, without conductive virus, a dead covid 19 vaccine, very traditional. More than 15 million inhabitants have benefited from Covaxin.
An article signed by six Indian doctors reminds us of the obvious and shows how Indian choices are poles apart from those of the West. It is taken from the blog of Jean-Pierre Kiekens, an Oxford graduate and former university professor, featuring news and independent political analysis of the pandemic with a focus on treatments.
The ICMR (Indian Council for Medical Research) was the first national research agency in the world that not only understood the importance of primary care in taming this pandemic, but also recommended treatment with specific drugs and treatment regimens. identified for each grade of Covid-19 patients. . It was a masterstroke that none of the overseas agencies including CDC (US), NHS (UK) and others were able to deliver.
All medical authorities continued to say there was no early treatment available to treat mild cases at home, but continued to increase hospital beds and ventilators that continued to fall short.
On January 30, 2021, India completed a year since the first case of Covid-19 was detected in India from Kerala. At the start of the pandemic, India as a country was very vulnerable to a major coronavirus outbreak. India is not only the second most populous country in the world, but it has some of the most congested cities with an average population density of around 470 people per km2. Add to that the lack of an already overburdened robust health infrastructure. From the start, many experts in Western countries predicted disaster for India. The US-based Center for Disease Dynamics and Economic Policy (CDDEP) said in its April 20 report that the total number of SARS-CoV-2 infections in India through September 2020 could reach 1 , 11 billion,
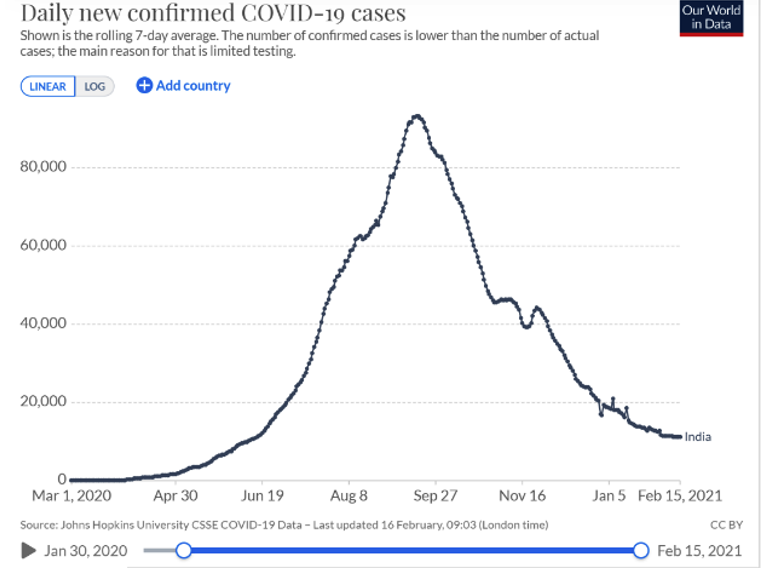
Cases in India increased steadily from April to September 2020, peaking at nearly 100,000 cases per day on September 16. Hospitals were filled to capacity and patients had to be turned away due to lack of beds; admissions were not guaranteed even for severe cases. Then things took an unexpected turn. Daily cases in India fell from mid-September to January, with average weekly cases declining by about a third each month. India currently reports around 10,000 cases per day on average. Hospital beds created for this purpose are now in excess and several Covid-19 facilities in large cities have been closed.
the herd. the community.
.
The herd immunity threshold depends on R0, (R null) which was close to 2 at the start of the transmission phase in India (March / April 2020) but dropped dramatically over the next few months and then reduced to less than 1 in September 2020 as shown in the graph below.

indicating a decrease in the rate of disease spread.
When R0 drops below 1, each infected person will (technically) infect less than one person.
At this rate, the disease eventually died out.
To confirm that R0 <1 means obtaining collective immunity, we can calculate mathematically using the following formula to estimate the threshold;
1-1 / R0.
In this case 1-1 / 0.97 = -0.03 (negative 3% instead of positive 60% for R0 of 2.5).
What has India done differently to reduce R0?
It is revealing to explore how this happened in India, but not in other countries where multiple waves continued to arrive within the same community despite country closures.
Take the United States and the United Kingdom as examples. The two countries have mainly focused on preventing the spread of the virus and have taken action accordingly. Their home treatment guidelines for asymptomatic cases were to wait 14 days in home isolation and, for mild cases, to treat symptoms with regularly available medications such as vitamins and minerals.
India, on the other hand, faced a daunting challenge with high population density and inadequate screening and health care facilities in the early stages. India had only 14 testing labs for Covid-19 as of February 2020, which was increased to nearly 1,600 in August 2020. Contact tracing efforts have been stepped up and contacts have been subject to ” rigorous follow-up to ensure almost complete coverage of cases. Given the burden on hospitals , the decision was made to treat asymptomatic and mild cases at home and moderate and severe cases in hospitals.
Therefore, the treatments recommended by the ICMR have been shown to be useful for the early treatment of patients at home. Since the country was on lockdown, there was a need to provide telemedicine guidelines for people to see their primary care doctors over the phone. The Ministry of Health then simplified and liberalized its telemedicine guidelines at the end of March to adapt them to the new model. These interventions took place from the first few months, which led to a drop in R0 from April itself as shown in the graph on the previous page.
Could aggressive first-line treatment as directed by ICMR have slowed the spread of infection? To verify this, we looked to sales of HCQ (Hydroxychloroquine) during this period, as recommended by the government. If we could convert the units to the number of patients treated and compare to the prevalence of Covid-19, we could get a correlation. Although not in the ICMR guidelines, we have decided to add ivermectin as the most populous state of UP declared for large-scale use in government health centers.
Sales of hydroxychloroquine and ivermectin in India to project the number of patients:
A compilation of HCQ data based on IQVIA sales figures (in addition to government sales as reported in the press) for the period April 2020 to December 2020 to project the number of patients who received it.



Interpretation:
- It looks like 29 mil. patients received HCQ during the period March to December 2020.
- Overlapping this 29 mil, 10.2 mil pts were PCR + five cases (or part of it) indicating that behind each + five case, approximately 2 other patients were also treated with HCQ. These may be close contacts, untested users, or people on prophylaxis.
- Patients taking ivermectin account for 56% of RT-PCR positive cases. However, like the state of UP which replaced HCQ with ivermectin, we assumed an overlap of only 50% with HCQ increasing the number of patients receiving either drug.
- This would project the number of patients receiving HCQ or Ivermectin to be over 30 mil (29 mil + half of 5.75 mil)
So, it’s safe to assume that behind every positive case of Covid-19 in India, there was some 2 others who received HCQ or Ivermectin.
Due to the hype around HCQ and Ivermectin, it is possible that part of the sales is due to the storage of these drugs at home / by organizations etc, around 10%. Even though the above projections are reduced by 10%, it remains at 27 million with a usage ratio of 2.7: 1 indicating overuse beyond positive cases.
These figures reflect an aggressive early treatment approach for mild / moderate cases using the above 2 drugs going beyond PCR + five cases. Correlated with the decline in R0 which led to the decline in new cases month-to-month, it appears to have played a major role in control in India. These interventions could very well precipitate the early establishment of herd immunity in India.
Related: Hydroxychloroquine & Covid-19: India and France, a cruel comparison
Act early with early Covid-19 treatment: Dr Vladimir Zelenko
The lawyer who won the Ivermectin battle for South Africans
Ivermectin is effective for COVID-19: real-time meta analysis of 42 studies
Shutdowns instead of hydroxychloroquine: The destruction of France is escalating