SOURCE: The Economic Standard Editor Erik Yass
Full PDF of report from source: HCQWhitePaper
EDITOR’S NOTE
This paper was written in close collaboration with practicing physicians and infectious disease specialists from across the United States and around the world. We are extremely grateful for their help in ensuring the accuracy of our analysis; any mistakes are The Economic Standard’s alone.
Erik Sass
Editor-in-Chief
OVERVIEW
The COVID-19 pandemic struck America nine months before a presidential election, turning basic medical activities like
testing and treatment into partisan battlegrounds. No subject has been more distorted than hydroxychloroquine (HCQ), a
safe, versatile medicine that has treated hundreds of millions of people for numerous diseases for seven decades.
HCQ was adopted as a COVID-19 treatment in Asia in January 2020 without fanfare, based on lab tests with the
related coronavirus SARS-1. But when President Trump stated in March that the U.S. would also begin studying the
drug’s potential against the virus, political opponents defied longstanding scientific and medical consensus to portray
HCQ as harmful and Trump as a mortal danger to public health. Flawed and even falsified studies were published and
promoted by media outlets eager to discredit Trump, while positive studies were impugned or ignored.
This campaign persists even as evidence of HCQ’s benefit against COVID-19 grows – including scores of
observational controlled trials showing therapeutic effect when administered early in disease progression. Hundreds
of drugs have been approved for both indication-specific and general usage on the basis of similar observational
trials, especially when conducted in large numbers and subject to careful meta-analysis. As a matter of medical
practice and especially in a pandemic emergency, it is flatly not the case that only randomized controlled trials can
justify adopting a treatment, as HCQ detractors have insisted while publicizing randomized controlled trials results
that are themselves deeply flawed.
The U.S. is an international outlier on HCQ. Right now, doctors around the world are prescribing HCQ to treat
COVID-19 outside of hospitals, as well as prophylactically to prevent infection among healthcare workers and
vulnerable populations. This paper argues that HCQ has met the appropriate burden of proof and urges members of
the U.S. news media, public health community, and regulatory agencies to stop politicizing the use of this medicine.
Tens of thousands of lives still hang in the balance.
INTRODUCTION
The novel coronavirus COVID-19 was identified in Wuhan, China in December 2019. Its rapid spread challenged
governments and tested healthcare systems around the world. The immediate concern was the absence of effective
treatments, prompting scientists and infectious disease specialists to scour pharmacological databases and research
archives for potential remedies. A number of promising candidates were identified, but no cure had emerged by the
time a local outbreak began in New York City in March 2020.
With lockdowns looming, President Trump first publicly mentioned HCQ during a press conference on March 19,
2020, alongside other hopeful treatments such as remdesivir. This was the first time most Americans heard of any of
these drugs. Speaking off the cuff, Trump stated:
“Now, this is a common malaria drug. It is also a drug used for strong
arthritis… And it’s shown very encouraging – very, very encouraging early results… I think it could be a game changer. And maybe not.”
Trump later added that the drug was considered safe and widely available – and indeed it was. As the following
timeline shows, these hopeful statements were in line with global medical opinion at the time, and supported by a body
of clinical evidence that has continued to grow. But that’s not how they were presented.
Instead, within days of Trump’s first mention of HCQ, the narratives that would shape media coverage emerged
centering on alleged dangers for patients and lack of efficacy against the novel coronavirus. These narratives were
constructed almost entirely in contradiction to facts. They ignored both the drug’s long history of safety and its already
widespread use in Asia and Europe as a treatment for COVID-19.
Understanding HCQ’s origins as a treatment for COVID-19 requires delving into the foundations of medical science
and retracing events in the rest of the world.
WHAT IS HYDROXYCHLOROQUINE?
As the suffix “-quine” indicates, HCQ belongs to a family of drugs based on quinine, the original antimalarial drug.
Indigenous South American tribes extracted it from the bark of the Cinchona tree, and used it to ward off the mosquitoborne parasitic disease. Western medicine first encountered quinine as early as the 17th century. French scientists discovered how to extract pure quinine from the bark in 1820, but the search continued for over a century for an easily manufactured form of the drug which could be administered on a large scale.
Finally, in 1934, researchers with German pharmaceutical giant Bayer synthesized chloroquine, a quinine derivative and predecessor of HCQ. During the Second World War, the German Army used a chloroquine analogue, Sontochin, for malaria prophylaxis. Sontochin then fell into Allied hands, and chloroquine was prescribed for malaria prophylaxis in America starting in 1947. The drug was so effective that the U.S. Army adopted chloroquine phosphate as standard malaria prophylaxis in 1962. Hundreds of thousands of American soldiers took the drug regularly in Korea and Vietnam.
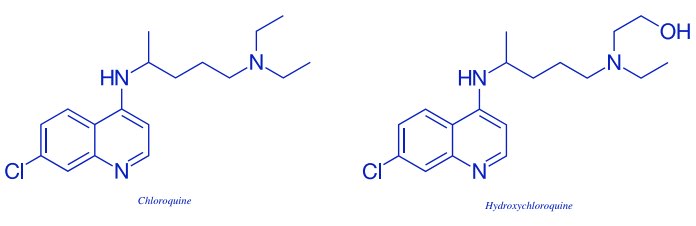
While chloroquine was clearly effective as an antimalarial, concerns about potential toxicity spurred the development of an even safer version. In HCQ, the chloroquine molecule is “hydroxylated” through the addition of a hydroxyl group (an oxygen atom bonded to a hydrogen atom). This makes the drug’s metabolites water-soluble for excretion in urine, thereby lowering its potential to harm. Following its development in 1946, HCQ played an important role in the
rapid elimination of malaria from the United States in 1947-1951.
The conquest of malaria in the U.S. didn’t spell the end of the drug, however. Beginning in the 1950s, medical researchers discovered that HCQ also possessed powerful anti-inflammatory and immunomodulatory properties. It suppresses cytokine signals in the
immune response, making it an effective treatment for a number of ailments besides malaria, including complex autoimmune conditions like rheumatoid arthritis and lupus.4 HCQ was also found to have
antiviral characteristics, hindering the reproduction of a number of major classes of virus. Today it is used to treat a remarkably diverse array of dermatological, immunological, cancerous, and infectious diseases.5,6
Scientists continue to explore the drug’s potential
against a wide range of other diseases, including HIV, hepatitis C, soft tissue sarcoma, melanoma, breast cancer, lung cancer, ovarian cancer, pancreatic cancer, Crohn’s Disease, Hashimoto’s thyroiditis, Hand Foot and Mouth Disease, and cystic fibrosis, as well as for thrombosis prevention and post-surgical wound recovery.
These long lists of current and potential uses demonstrate HCQ’s unusual versatility and wide range of action. They also reflect a general medical consensus,
long predating the COVID-19 pandemic, that HCQ is a safe, well-tolerated drug.
CONDITIONS OTHER THAN MALARIA
FOR WHICH HCQ IS INDICATED OR
COMMONLY PRESCRIBED
• Discoid lupus
• Systemic lupus erythematosus
• Rheumatoid arthritis
• PCT and chronic ulcerative stomatitis
• Hepatic amoebic abscess
• Refractory chronic urticaria
• Dermatomyositis
• Sarcoidosis
• Polymorphous light eruption
• Disseminated granuloma annulare
• Sjögren’s syndrome
• Erosive lichen planus
• Frontal fibrosing alopecia
• Necrobiosis lipoidica
• Chronic actinic dermatitis
• Actinic reticuloid
• Actinic prurigo
• Epidermolysis bullosa
• Kikuchi–Fujimoto disease
• Graft-versus-host disease
• Chronic erythema nodosum
• Morphea and systemic sclerosis
• Pemphigus vulgaris
• Pemphigus foliaceus
• Pemphigoid gestationis
“AN EXTREMELY SAFE DRUG”
The American news media’s fearful reaction to Trump’s mention of HCQ in mid-March was completely at odds with the longstanding medical consensus that the drug is safe for general use with straightforward precautions. That consensus was based on hundreds of scientific studies and the experiences of millions of patients. Among other things, the drug’s safety is clearly reflected in pre-pandemic guidance issued by U.S. and global health agencies.10
Like most drugs, HCQ has potential side effects. The most common ones, gastrointestinal disturbances, are largely minor. Some are dangerous but extremely uncommon. The most potentially serious side effect associated with HCQ is QT prolongation, a change in the heart muscle’s electrical signaling system. This change raises the risk of “torsades de pointes,” an abnormal heart rhythm which can (very rarely) result in sudden death. QT prolongation is itself a temporary, reversible side effect experienced by about 10% of patients, of whom some may need to stop taking the drug if the prolongation is sufficiently severe. However, if there is an indication to do so, QT prolongation is easily detected with appropriate monitoring by EKG, and doesn’t preclude use of the drug on an outpatient (nonhospitalized) basis. Small amounts of QT prolongation are considered allowable and are the most common form of this change, when the change is seen at all. HCQ’s degree of QT prolongation puts it in the midrange of 30 commonly used drugs. Some major drug classes, such as fluoroquinolones, result in far more pronounced QT prolongation than HCQ but are still widely used.

The essential safety of chloroquine and HCQ is reflected in the vast scale of the drugs’ historic usage, with tens of billions of doses consumed by many hundreds of millions of people over seven decades. These were mostly for the treatment of malaria and virtually all outside the hospital setting and without screening EKGs. From 1978-1988 world consumption of chloroquine exceeded 3,000 metric tons, equal to about 14 billion doses over that decade alone.12 In 2005 it was estimated that annual consumption of chloroquine for treatment of malaria was still in the range of 300-500 million courses per year, despite the rise of chloroquine-resistant malaria.13 In the U.S. alone from 2007-2017, patients received around 59 million prescriptions for HCQ. This includes some 1.5 million people living with autoimmune diseases like lupus or rheumatoid arthritis, who are typically prescribed two 200 mg pills daily for a period lasting years.14,15,16
By all accounts the incidence of torsades de pointes resulting from heart arrhythmia is extremely low. In over seven decades of use, there have been a handful of reports of fatal arrhythmias due to torsades de pointes from all drug causes, and zero reports of fatal arrhythmias with HCQ use.17 Most cases of arrhythmia involved extraordinary circumstances, including overdoses and patients with end-stage liver failure. Other side effects, such as retinopathy and kidney damage, result only from years of long-term use and have been described as “rare.”18
A 2014 study found no adverse long-term effects of HCQ in the children of women with systemic lupus erythematosus. The study investigator, Dr. Mary Gayed of the University of Birmingham’s department of rheumatology concluded that, “Hydroxychloroquine should be continued during pregnancy and breastfeeding.”19
The pre-pandemic medical consensus on the safety of HCQ is summarized in this advice for patients, published by the Rheumatoid Arthritis Support Network in 2018:
“Like all medications, there is the risk of side effects. Fortunately, the problems seen by people taking this medication are usually very mild. Serious side effects are rare. Overall, most people who have any noticeable side effects from hydroxychloroquine experience diarrhea or nausea. These usually get better after the person adjusts to the medication, and taking the drug with food can help, as well. Additionally, some people experience anemia and vision changes or even vision loss, but this is quite rare. It’s more commonly seen with high doses for long periods, in older people, and in those who have kidney problems.”20
Hydroxychloroquine is sometimes administered in combination with azithromycin, another drug which sometimes prolongs QT. This much-discussed drug pairing is estimated to produce fatal arrhythmias in roughly nine out of 100,000 patients receiving it, or 0.009% of subjects – which presumably would be even lower with appropriate
monitoring.21 This author notes that, “fatal arrhythmia outcomes are so rare that they are of much lesser clinical significance than the hospitalization and mortality that the drugs prevent.”22
SAFETY OF HCQ AND CHLOROQUINE
“Hydroxychloroquine can be prescribed to adults and children of all ages. It can also be safely taken by pregnant women and nursing mothers… Hydroxychloroquine is a relatively well tolerated medicine.”
– Patient fact sheet, Centers for Disease Control23 “If it is taken in proper doses, chloroquine is an extraordinarily safe drug.”
– Ilan Ben-Zvi, et al. “Hydroxychloroquine: From Malaria to Autoimmunity.”24
“Antimalarial medications are extremely safe…”
– Patient fact sheet, Rheumatic Dermatology Society.25
“Chloroquine and especially HCQ are considered very safe medications.”
– Ronald F. van Vollenhaven, “Systemic Lupus Erythematosus: Which Drugs and When?”26
HCQ VS. COVID-19
Facing a global pandemic, with ICUs overflowing and death tolls soaring, healthcare providers around the world urgently sought potential weapons to fight the novel coronavirus. Many judged HCQ’s limited side effects an acceptable risk in that context. Today, notwithstanding American controversy, dozens of countries continue to use HCQ for COVID-19 treatment and prevention. In fact, a quick review of the timeline reveals that the U.S. is an international outlier on HCQ, as one of just a handful of countries that have moved to limit – rather than expand – patient access to the drug.
While parts of the story remain unclear, the origins of HCQ as a treatment for COVID-19 date back to January 2020, when Chinese doctors in Wuhan reportedly screened databases of existing drug molecules and identified HCQ’s predecessor, chloroquine phosphate, as a possible candidate based on its antiviral properties. These included laboratory tests backed by the CDC from 2004-2009 showing inhibition of the reproduction of the original SARS coronavirus – a close relative of COVID-19.27 By early February, doctors in Wuhan claimed that in vitro research28 and observational evidence from clinical usage in patients29,30 indicated chloroquine and HCQ were effective against COVID-19. On February 15, HCQ was included in the sixth version of the COVID-19 treatment guidelines issued by the National Health Commission of the People’s Republic of China at Wuhan.31 These early findings were reported in global publications as early as February 6.32

As the disease fanned out across the world, interest in chloroquine and HCQ as treatments for COVID-19, frequently
in combination with other drugs, also spread to neighboring countries. South Korea detected its first case on January 20. By February 8, that country was already considering chloroquine or HCQ as a treatment for COVID-19.33 On March 12, a week before Trump’s first mention, South Korea’s version of the CDC officially recommended HCQ, in
combination with lopinavir and ritonavir, as a treatment for COVID-19.34
South Korea’s adoption of HCQ35 was soon emulated by other national and regional health authorities. The drug was quickly authorized to treat COVID-19 in France,36 Spain,37 Italy,38 and Turkey.39 Malaysia began using chloroquine against COVID-19 during the first wave of the disease there in January and February.40 Bahrain began using it on February 26, and Poland approved a chloroquine-based drug for COVID-19 on March 13. HCQ was also authorized
to treat COVID-19 or incorporated into standard of care in Russia, Iran, Egypt, Pakistan, India, and the Philippines, among many others.41
In many of these places doctors prescribed HCQ on an outpatient basis,42 as well as prophylactically, to prevent infection among healthcare workers and vulnerable populations. American health regulators have discouraged both of these uses. Indian health authorities claimed to have prevented COVID-19 infection among healthcare workers with mass prophylaxis,43 and South Korean doctors reported success with HCQ prophylaxis among nursing home patients who had been exposed to COVID-19.44
OBSERVATIONAL STUDIES
VS. RANDOMIZED CONTROLLED TRIALS
These were several among a growing number of positive clinical research findings supporting the use of HCQ, and some American doctors expressed support for the drug on this basis.45 However, most of these early findings came from observational controlled trials or retrospective controlled studies rather than randomized trials. This distinction has become a central pillar of the media narrative about HCQ, based on the mistaken premise that only randomized controlled trials (RCTs) provide sufficient evidence for the use of a drug to treat a particular condition. This premise is at odds with current practice and the history of medical science. In fact, hundreds of drugs have been approved for both indication-specific and general usage on the basis of observational trials, including azidothymidine for HIV/AIDS and insulin for diabetes, and this practice has continued in recent years.46
So what is the difference between RCTs and observational trials? In randomized controlled trials, the efficacy of a potential treatment is determined by using a computer to randomly assign patients into two groups: an experimental group which receives the drug, and a control group which receives either the standard treatment (where one exists) or a placebo. When these trials are “double-blinded,” neither the prescribing doctor nor the patients know whether they are receiving the experimental drug or the placebo. This limits the potential for physician bias in deciding who receives the drug and their subsequent care.
In observational trials, which dominated medical science for most of its history, doctors observe outcomes of patients taking a particular drug, then try to judge efficacy by comparing them with a control group of people who didn’t receive the drug. There are various methods for defining control groups. In some, patients are provided with informed consent and then choose whether or not to take the drugs. In others, doctors recommend which treatment they think will be best for each patient.
Because drug assignment is not randomized, observational studies can be more open to bias compared to RCTs. This is called “confounding by indication,” which means the reasons why certain patients did or did not take the drug may influence the study outcome as much as, or more than, the effects of the drug itself. For example, a doctor may unconsciously choose to give the drug to patients who are less sick, yielding more positive results. Conversely, a doctor worried about potential side effects might hold off until patients are already very sick, producing a negative bias.
However, it’s important to note that medical researchers have developed ways to account for possible biases in observational studies, by controlling for other reasons that the trial may be yielding a particular result. In the case of drug efficacy studies, these “confounding factors” can include a range of patient characteristics and treatment modalities. For example, when comparing treated versus untreated patients, researchers make sure that the patients in each group are as close to each other as possible in terms of baseline characteristics such as age, sex, and severity of illness. One such technique, propensity score matching, involves taking patients from each group and matching them for as many variables as possible.
DRUGS & TREATMENTS APPROVED
WITHOUT RCTS
• Tetanus vaccine
• Insulin
• Hydrocortisone
• Tetracycline
• Clindamycin
• Warfarin (Coumadin)
• Heparin
• Prednisone
• Methylphenidate (Ritalin)
• Thorazine
• Glucagon
• Amitriptyline
• Furosemide (Lasix)
• Keflex
• Monistat
• Azidothymidine
• Cyclophosphamide (Wegener’s
granulomatosis)
• ZOSYN (piperacillin-tazobactam
combination)
• High-dose IV penicillin for neurosyphilis
• Vancocin (IV vancomycin)
• Aqueous penicillin g potassium
• Amoxil (amoxicillin)
• Avycaz (ceftazidime/avibactam)
• Merrem (meropenem)
Armed with these techniques, careful researchers can derive meaningful results through observational studies. In fact, meta-analyses – studies which review a large number of previous studies with statistical methods – have shown that in many cases observational studies can anticipate the results of RCTs years in advance. This is especially true when large numbers of observational studies are performed and analyzed in the aggregate, as errors and biases are less likely to distort the results of large-scale comparisons.
One sweeping meta-analysis, drawing data from seven databases, compared more than 1,000 pairs of observational studies and RCTs across 228 medical conditions. It concluded that “on average, there is little evidence for significant effect estimate differences between observational studies and RCTs, regardless of specific observational study design, heterogeneity, or inclusion of studies of pharmacological interventions.”47 Another group of authors concluded that “the average results of the observational studies were remarkably similar to those of the randomized, controlled trials.”48 A third meta-analysis, reviewing 136 studies of 19 treatments, concluded: “We found little evidence that estimates of treatment effects in observational studies…are either consistently larger than or qualitatively different from those obtained in randomized, controlled trials.”49
In short, while any individual observational study may be better or worse conducted, it is highly misleading to portray observational studies generally as merely “anecdotal.” Again, many of today’s commonly used treatments were discovered or validated through careful observational trials and only later, if ever, subject to RCTs. It should also be emphasized that this practice continues. A review of cardiac drug approvals and treatment recommendations from 2008-2018, covering 51 current guidelines, found “the proportion supported by evidence from RCTs remains small,” including just 8.5% of American College of Cardiology/American Heart Association (ACC/AHA) guidelines and 14.3% of European Society of Cardiology (ESC) guidelines.50 On that note, another review of observational studies and RCTs argues: “We do not believe that dependable clinical evidence only comes from RCTs….If RCTs were required for proof of efficacy of a given treatment, the practice of clinical medicine would indeed be reduced to a relatively few verified treatments.”51
Government regulatory agencies in the U.S. and across the world routinely use observational study evidence to make inferences about causal outcomes. The foundational method for such work was laid out in 1965 by Sir Austin Bradford Hill. He identified nine “aspects” of causal reasoning evidence that in sum provide a rationale for deducing causation. To this day the aspects identified by Hill remain the most widely used framework for general causal reasoning across medicine, science and law. One of these aspects is “experiment,” which includes RCTs, but these comprise only a small component of causal evidence. Hill’s main point is that all forms of scientific evidence must be considered and weighed, with no single type considered solely definitive.52
It’s particularly unrealistic to demand RCTs confirming HCQ’s efficacy against COVID-19 before using it for that purpose for a number of reasons. Ethical considerations play a role, as some healthcare providers might refuse to carry out RCTs during a pandemic because it requires knowingly giving ill people a placebo or putatively less effective medication. RCTs also face logistical challenges. High-quality randomized studies require intensive preparation, controls and oversight. These expenses are often beyond the limited resources available in many healthcare settings, especially in low- and middle-income countries. And poorly designed and executed RCTs can just as easily produce results that are meaningless or misleading – as has been the case with HCQ and COVID-19, as shown below. In fact, science theorists have argued that “in the end, an observational study with credible corrections and a more relevant and
much larger study sample…may provide a better estimate [than small or flawed RCTs].”53
“When conventional care means such a high probability of death, it is
problematic to insist on randomising patients to it when the intervention arm holds out at least the possibility of benefit. Ethical arguments are not the same for all levels of risk.”
– Adebamowo C., Bah-Sow O, Binka F, et al. “Randomised controlled trials for Ebola: practical and ethical issues.”54
Given the ethical and logistical constraints imposed by the COVID-19 pandemic, it would be difficult, if not impossible, to organize and implement high-quality RCTs in the time available. This means that decisions about HCQ and other drugs necessarily have to be based on the results of observational studies, which, again, have yielded hundreds of useful drugs and guided medical decision over many decades.
This process is in line with precedents established in previous epidemic emergencies, including the first SARS epidemic and 2014 Ebola epidemic. There, public health policy makers authorized clinical use of unproven treatments like lopinavir, ritonavir, favipiravir, ribavirin, and interferon – without RCTs – due to urgent need amid insurmountable logistical and time constraints.55,56
Thus, as a matter of medical practice and especially in a pandemic emergency, it is flatly not the case that only RCT demonstration can justify adopting a treatment. Observational trials, meta-analyses and evidential reasoning along Hill’s aspects, properly conducted, can serve to meet the burden of proof appropriate for adoption, as a matter of science and public-health policy. The opposition to HCQ as a treatment for COVID-19 has largely ignored these basic facts.
HCQ’S EFFICACY BASED ON CONTROLLED
OBSERVATIONAL TRIALS
A substantial body of data has accumulated supporting HCQ in the treatment of COVID-19. This includes scores of controlled observational trials subjected to meta-analysis, as well as a modest number of small-scale RCTs. Across the board, these studies suggest that HCQ is in fact effective in saving lives, lessening symptoms, and shortening recovery time – when it is used early in the disease process in appropriate doses. A typical course of HCQ treatment for COVID-19 treatment is that advised by the Indian public health service, calling for 400 mg twice on day one, followed by 400 mg daily for the next four days.58,59,60
Observational studies subject to careful meta-analysis show strong support for HCQ as a COVID-19 treatment. An ongoing meta-analysis of 102 HCQ studies conducted in the U.S. and abroad (including 61 peer-reviewed, most of them observational) concludes: “PrEP, PEP, and early treatment studies show high effectiveness, while late treatment shows mixed results.” The study authors (https://c19study.com/) provide a lengthy explanation of their sources and methods for dealing with biases in the study set, as well as detailed commentary on the strengths and weaknesses of the individual studies.61
A separate meta-analysis of 26 clinical and “Big Data” studies concluded that “chloroquine derivatives are effective to improve clinical and virological outcomes. But, more importantly it reduces mortality by a factor of three in patients infected with COVID-19.”62 A third meta-analysis covering 43 studies concludes: “HCQ was found consistently effective against COVID-19 when used early, in the outpatient setting,” adding, “No credible study found worse outcomes with HCQ use. No mortality or other serious safety issue was found.”63
A study at the Henry Ford Health System based in Detroit considered 2,541 mostly older, African-American patients, who were treated early in-hospital with HCQ (paired in some cases with azithromycin). This study found that “Hydroxychloroquine provided a 66% hazard ratio reduction, and hydroxychloroquine + azithromycin 71% compared to neither treatment.” The study matched treated and nontreated subjects on steroid use and other variables and still showed significant treatment benefit. Addressing the risk of QT prolongation, the authors further noted that “no patient had documented torsades de pointes.”64
Another large study of COVID-19 patients treated with HCQ during the first 24-48 hours at four NYU hospitals, analyzed using multivariate statistical methods, found that a similar drug combination decreased mortality and increased likelihood of discharge, adding that it performed best when used early in disease progression: “The decrease in mortality or transition to hospice was most striking when considering only patients who were not admitted to the ICU.”65
Yet another observational study of more than 1,000 COVID-19 outpatients in New Jersey, which used propensity score matching to control for bias, found a significant positive effect for use of HCQ in preventing hospitalization: “In a 1,067 patient propensity matched cohort, 21.6% with outpatient exposure to hydroxychloroquine were hospitalized, and 31.4% without exposure were hospitalized.” On the safety issue, the authors add: “QTc prolongation events occurred in 2% of patients prescribed hydroxychloroquine with no reported arrhythmia events among those with data available.”66
Comparative disease statistics also reveal a significant trend. A continuing analysis shows that countries that adopted early treatment with HCQ have an average adjusted mortality 78% lower than among those that did not (157.4 per million versus 714.6 per million).67 Country-level statistical analyses also support HCQ’s efficacy against COVID-19: data from Switzerland shows a distinct rise in mortality among COVID-19 patients when HCQ was briefly withdrawn in late spring following the retracted Lancet study.

A POSSIBLE MECHANISM OF ACTION
FOR HCQ AGAINST COVID-19
While it may take decades of work to untangle HCQ’s precise mechanism of action against COVID-19, experts have already begun assembling a theoretical framework based on clinical observations and laboratory studies.68 Though speculative, this framework may also account for some of the disease’s characteristics.
Under one theory, SARS-CoV-2, the virus that causes COVID-19, first infects tissues of the nose and mouth. If a strong innate immune response can be mounted at this point (non-specific dendritic cells, T cells, macrophages), the virus is cleared after a few days with only mild upper respiratory symptoms.69 If this initial immune response is weaker (as in the elderly or those with immunodeficiencies) and/or if the viral load is high, the virus is not cleared, and can travel deeper to the lungs through aspiration of nasal mucus containing virus to
these lower lung areas. It is here in the lower lungs that a strong adaptive (antibody B cell and cellular T cell) immune response can happen. This response begins to peak about 7-10 days after the onset of symptoms, and can lead to cytokine storm and acute respiratory distress syndrome (ARDS) if unchecked.70
HCQ has multiple proposed mechanisms of action which can interact with this disease process, many of which have been confirmed in cell culture and in human studies. It can strengthen the early innate immune response to the virus in the nose and mouth through boosting of the immune response of a particular master immune cell, called a dendritic cell, to viral proteins (antigens). This allows stimulation of specific T cells called cytolytic CD8 cells against the virus in the nose and mouth, and can help to limit the viral infection to these areas.71
The virus also requires several steps to enter host cells, including cleavage of the viral protein spike in cellular structures called endosomes and lysosomes, by enzymes called furins and cathepsins.72 HCQ blocks the movement of the virus through the cell to the lysosome, and when given with zinc also likely blocks the
activity of the furin and cathepsin enzymes.73 Therefore, HCQ can reduce productive viral infection of host cells. For the reasons above it appears to be important to give HCQ early, to limit viral infection to the nose and mouth, and to reduce viral load there to prevent spread to others though coughing and sneezing.
HCQ can also modulate the activity of the adaptive immune response later in the course of SARS-CoV-2 infection, after the virus has spread to the lower lung of susceptible individuals. HCQ reduces activity of immune cells called macrophages. These cells are stimulated to attack by antibodies binding the virus in the lower lung. They become polarized to an inflammatory state called M1, and secrete factors called cytokines which can lead to cytokine storm and ARDS.74 HCQ can prevent this polarization of macrophages to the inflammatory M1 state and convert these macrophages to a milder “wound healing” M2 type, which does not secrete inflammatory cytokines.75
If given before the adaptive immune response in the lower lung has had too much time to build, HCQ can therefore blunt this response, lower inflammatory cytokine levels, and possibly prevent cytokine storm and ARDS. This is why HCQ may need to be given earlier in a hospitalization or on an outpatient basis. If given too late, especially if a patient is near intubation or has been intubated, the immune response may already be too strong for HCQ to work. This is likely why the results of trials of HCQ in hospitalized inpatients have been
so mixed. Those that consistently give the drug early (within 24-48 hours of hospitalization) appear to have positive results, and those that give the drug later do not.
HCQ’s wide range of action means that it is probably interacting with the disease process in a number of ways. For example, uncontrolled high glucose levels in hospitalized inpatients appear to result in increased mortality, and HCQ is a hypoglycemic agent that reduces glucose.76 Increased blood clotting in severe coronavirus pneumonia can lead to poor outcomes through pulmonary embolus and stroke, and HCQ also reduces such blood clotting.77 Zinc, in the presence of such an ionophore, shows potent anti-viral activity in vitro and possibly in animal models and in humans against coronaviruses.78
Therefore, there are multiple possible theoretical mechanisms by which HCQ can work to ameliorate coronavirus infection and pathology. The need to give HCQ earlier in the disease course, based on these mechanisms, likely explains a great deal of the confusion concerning the mixed results of HCQ trials in COVID-19 infection.
HCQ’S POLITICIZED RECEPTION
Despite the mounting evidence in favor of HCQ, the distinction between observational studies and RCTs created an opening for the politicization of the drug by the American news media. Reporters focused on low-quality or botched RCTs – misrepresenting these as the “gold standard” – while dismissing observational studies as irrelevant due to supposed biases. Exploiting the public’s lack of knowledge about the scientific process, news outlets crafted an
inaccurate and misleading narrative about HCQ’s alleged dangers and supposed lack of efficacy against COVID-19. This narrative was sustained and amplified by scientists, academics, and government agency staff. For the purpose of this paper, we will focus our attention on media narratives where each of these actors played a role in validating and amplifying bad science.
A review shows the central media narratives designed to discredit the drug centered on two main supposed concerns: alleged dangers to patients, and lack of efficacy against COVID-19. The main aim of these narratives was to label the drug as unsafe and ineffective.79 However, neither narrative stands up to scrutiny.
The most serious media mischaracterizations centered on HCQ’s safety, characterized by lurid anecdotes and wild exaggeration of the drug’s established side effects. For instance, the death of an Arizona man after ingesting aquarium cleaner containing chloroquine phosphate was blamed on the president, with CBS News reporting, “Arizona man dies, wife ill after taking drug touted as virus treatment,” quoting the man’s wife at length:
“I saw it sitting on the back shelf and thought, Hey, isn’t that the stuff
they’re talking about on TV?…Trump kept saying it was basically pretty much a cure,” she said, adding her advice for people would be, “Don’t take anything. Don’t believe anything. Don’t believe anything that the president says and his people…call your doctor.”80
This event would be cited time and again in the months that followed, as news media wove a narrative about HCQ’s supposed dangers. The Washington Post revisited the event a month later in a timeline purporting to chart “The rise and fall of Trump’s obsession with hydroxychloroquine”: “That evening, some grim news. A couple in Arizona ingested a substance called chloroquine phosphate, a medication for fish, under the mistaken assumption it would protect them from the coronavirus. One person died, the other was hospitalized.”81
The media narrative soon moved on to HCQ’s potential side-effects, which were amplified until a drug long used by
millions of Americans became virtually unrecognizable. The potential for QT prolongation among a small subset of patients, long judged an acceptable risk in the treatment of other ailments, became a “dangerous” and “deadly” threat in the context of COVID-19. Sensational reports attributed deaths to HCQ with no evidence,82 while Fox News TV anchor Neal Cavuto warned “it will kill you,” ignoring the drug’s record of no fatal arrhythmias in regular use.83
The deceptive reporting on HCQ was often nakedly political, making no secret of the intention to discredit Trump for promoting the medicine. A commentator for USA Today, citing the president’s mentions of HCQ, opined that “Trump’s coronavirus briefings are too dangerous for news media to show them live.”84 Other commentators cited Trump’s mentions of HCQ to call for his removal under the Twenty-Fifth Amendment, while The Hill reported that an Ohio lawmaker wanted to charge Trump with crimes against humanity in international tribunals because of them.85
Democrats who spoke favorably of HCQ were rebuffed. On April 6, Michigan state Representative Karen Whitsett, a Democrat representing Detroit, credited HCQ with her recovery from COVID-19 in March.86 She met with President Trump during an April 14 gathering of COVID-19 survivors and expressed gratitude for his promotion of the medicine, which is how she learned about it: “Thank you for everything that you have done… I did not know that saying thank you had a political line… I’m telling my story and my truth, and this is how I feel and these are my words.”87
Shortly after this on April 25, delegates of the 13th Congressional District Democratic Party voted unanimously to censure Representative Whitsett, barring her from the group’s activities for two election cycles.88
THE DATA GAME
The U.S. news media next sought to invoke science in its misleading political attack, readily promoting studies that showed negative outcomes for HCQ while attempting to discredit or ignoring positive data. Enabled and supported by low-quality science and scientific malpractice, the new narrative overwhelmingly emphasized the “unproven” nature of the drug because of the lack of RCTs, while dismissing as “anecdotal” the positive findings of observational studies.
The language adopted by the press was strikingly uniform. A Google News search for the words “unproven” and “hydroxychloroquine” in reports published in April and May returned over 160 results, with most of these articles managing to work the adjective into headlines or opening sentences. None of these reports mentioned that
observational trials had discovered useful drugs in the past. Nor did they clarify that many observational studies in aggregate can yield more meaningful results than any one single study, RCTs included.
Instead, journalists pointed to individual observational studies of other diseases as proof that observational studies overall are meaningless. One science writer declared “Again and again they [observational studies] have been wrong.”89 Another physician author dismissed observational studies as mere steppingstones to large-scale RCTs, with no real value in themselves: “Although often limited and flawed, observational studies are cheap and easy to complete. Their
real value is to drum up interest in performing larger randomized controlled trials.” The same author concluded with the now-familiar language equating observational studies with hearsay: “Life-and-death decisions in medicine cannot be left to simple observational studies or, even worse, anecdotal evidence.”90
At the same time, the major randomized clinical trials cited by HCQ critics were themselves of low quality and limited scientific value, in many cases reflecting the obvious constraints imposed by the pandemic.
Nearly all the RCTs completed to date have been “underpowered” – meaning they either dealt with a small group of subjects or failed to accumulate their enrollment targets – due in part to the climate of fear around HCQ. But underpowered patient enrollment was just one of a number of flaws undermining the most-cited RCTs, including changing metrics midstream and broad variations in dosages and timing, which together make these trials far less meaningful. The methodological shortcomings of these RCTs were highlighted and discussed in public scientific fora and reported in foreign news outlets. 91
FOUR PROBLEMATIC
RANDOMIZED CONTROLLED TRIALS
- A RANDOMIZED TRIAL OF HYDROXYCHLOROQUINE AS POSTEXPOSURE
PROPHYLAXIS FOR COVID-19
• Virtually total lack of PCR testing for COVID-19, with just 2.6% receiving standard tests, forcing
researchers to rely on subjective self-reporting of symptoms
• Treatment started an average of four days after COVID-19 exposure, rather than no later than two days
as recommended
• Included mostly low-risk individuals who generally do well without treatment
• Not blinded: healthcare workers received identifiable pills
• Study stopped prematurely, before statistically significant figures
• Reanalysis shows the statistical significance of the large benefit of early treatment, contrary to the
authors’ claims
Boulware, et al. “A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19.” N Engl J Med August 6 2020;
383:517-525. Doi: 10.1056/NEJMoa2016638
- HYDROXYCHLOROQUINE IN NONHOSPITALIZED ADULTS WITH EARLY COVID-19
• Underpowered, with 491 subjects recruited over the Internet versus designed for 6,000
• Lack of testing, leading to inclusion of patients with “probable COVID-19”
• Changing metric, beginning with hospitalizations but transitioning to symptomatic endpoints
• Study was not blinded to the participants
• Study used an active placebo medication (folate)
Skipper, et al. “Hydroxychloroquine in Nonhospitalized Adults With Early COVID-19.” Annals of Internal Medicine, July 16, 2020.
Doi: https://doi.org/10.7326/M20-4207
- HYDROXYCHLOROQUINE WITH OR WITHOUT AZITHROMYCIN IN MILD-TOMODERATE COVID-19
• Changed endpoint from viral load at day three to viral load at day seven
• Changed endpoint to symptomatic rather than PCR test
• Patient pre-trial medications not controlled
• Median time from symptom onset to randomization 7 days, too late for HCQ to have early
treatment benefit
Cavalcanti, Alexandre, et al. “Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19.” N Engl J Med July 23, 2020;
DOI: 10.1056/NEJMoa2019014
- EFFECT OF HYDROXYCHLOROQUINE IN HOSPITALIZED PATIENTS WITH COVID-19:
PRELIMINARY RESULTS FROM A MULTI-CENTRE, RANDOMIZED, CONTROLLED TRIAL
(“RECOVERY” TRIAL)
• Study was not a randomized trial; instead, the allocation of the drug was randomized, and the timing
of drug administration varied widely
• Study suffered from “confounding by indication”: patients who received HCQ were already
sicker than those who didn’t
• Used dosage far exceeding recommended 2800 mg over six days
Horby, Peter, et al. “Effect of Hydroxychloroquine in Hospitalized Patients with COVID-19: Preliminary results from a multi-centre, randomized,
controlled trial.” medRxiv, July 15, 2020. Doi: https://doi.org/10.1101/2020.07.15.20151852
A recent meta-analysis based on these flawed RCTs produced equally flawed results.92 Among its many shortcomings, the meta-analysis drew 87% of its statistical weight from the unsound RECOVERY trial discussed above, which used such high doses of HCQ it received ethical criticism for potential toxic overdosing (Horby).93 Further the meta-analysis’ data for outpatient treatment, a critical area for HCQ usage, included two other problematic RCTs (Boulware,
Mitjà) as well as a number of studies with fewer than 20 subjects each. These underlying defects render the meta-analysis based on these RCTs effectively meaningless.
In some cases RCT authors either ignored or misinterpreted data confirming HCQ’s efficacy, prompting other scientists to voice “concern that a significant part of the medical community, and specifically some articles in medical journals, are misinterpreting the statistical results in randomized clinical trials conducted so far to answer the question regarding the effectiveness of hydroxychloroquine in the early treatment of COVID-19.”94 In one example from Spain, an RCT which ostensibly claimed no benefit for HCQ (and was reported in news media as such) actually revealed that the drug had a large positive benefit among high-risk patients. Using test-positive infection after demonstrated exposure as an endpoint, the Spanish study showed that HCQ prophylaxis and treatment reduced the risk to a population of 293 elderly nursing home residents by half.95
In a clear-cut double-standard, the American press was also quick to cite low-quality observational studies, provided they presented a negative result. Once again, The Washington Post set the tone with an article titled, “Drug promoted by Trump as ‘game changer’ increasingly linked to deaths,” citing data from one observational (not randomized or placebo-controlled) study96 by doctors at a Veterans’ Administration hospital in mid-May.97 Citing the same study in
an article for New York Magazine, titled “Trump Takes Hydroxychloroquine, Does Not Understand How Science
Works”, Jonathan Chait claimed that “as more evidence has come in, using hydroxychloroquine has gone from silly to insanely dangerous.”98
These statements are demonstrably false. The VA study was flawed,99 encapsulating many of the errors associated with
studies cited by critics to give their rhetoric a scientific gloss. In the study, the choice of providing patients with HCQ was left to physicians. Unsurprisingly, the cohort of 90 patients receiving HCQ prior to intubation were much sicker than the group of 177 patients not receiving HCQ prior to intubation – a classic prescribing bias.
Additionally, the timing of the treatment was apparently left up to the physicians as well, and the number of patients dying with and without ventilation indicates heavy “cross-over” to HCQ after patients were put on ventilators, and therefore much sicker; in fact, 75% of the patients not initially receiving HCQ prior to intubation were subsequently started on HCQ late in the clinical course, after they had deteriorated and required intubation.
Despite the supposedly negative conclusions of the VA study, just 7.8% of the initial HCQ patients later had to be intubated, compared to 14.2% of the other 177 patients not on HCQ who required intubation. In short, HCQ actually appeared to reduce the risk of intubation by 50% – even with bias favoring the non-intervention group.
These concerns were shared with the VA study’s corresponding authors on April 27, 2020, but to date no reply or clarification has been forthcoming.
This is only one example of many such negative observational studies on HCQ that were reflexively promoted and sensationalized by the media, but which under careful review did not stand up to scrutiny.
FROM BAD SCIENCE TO MALPRACTICE
The shortcomings of major scientific studies cited by HCQ critics weren’t limited to low numbers, poor study controls, and changing metrics. The politically motivated campaign to discredit the drug extended to what can only be classified as scientific malpractice.
On May 22, The Lancet published a multinational registry analysis spanning 671 hospitals on six continents, concluding that HCQ not only didn’t help COVID-19 patients but increased their chance of death.100 The study was widely reported as the final nail in the coffin for HCQ.101 The World Health Organization along with several
countries immediately suspended clinical trials with the medicine.102
Within a short time independent scientists identified problems with the study – noting that the journal had violated its own ethical guidelines in the rush to publication without verifying the underlying data – and circulated an open letter questioning its conclusions.103 Among other things, these authors noted “inadequate adjustment for known and measured confounders,” lack of ethics review, no data sharing, and “no mention of the countries or hospitals that contributed to the data source and no acknowledgments to their contributions.” They further noted that data ostensibly sourced from Australia was “not compatible with government reports.”104 The Lancet launched an independent investigation, and when the study authors refused to provide the underlying data, the study was retracted.105
But the damage was done. The Lancet’s publishing of misinformation gave public health regulators around the world a false scientific pretext to further limit access to HCQ. In the U.S. these measures were never reversed, even after the study was publicly withdrawn. This campaign of misinformation also succeeded in discouraging doctors from prescribing the drug and had a chilling effect on further enrollment in clinical trials, slowing the scientific process needed to determine the drug’s true efficacy. Even the National Institutes of Health halted its trial for the medicine under the pretense that, “while there was no harm, the study drug was very unlikely to be beneficial to hospitalized patients with COVID-19.”106
CONCLUSION
By systematically misrepresenting HCQ’s efficacy and safety for political ends, its opponents have deprived many tens of thousands of Americans of a potentially life-saving treatment and risk even more in the months and years to come. Members of the news media, public health community, and regulatory agencies must stop politicizing the use of this medicine. Properly powered RCTs can and should be conducted to confirm HCQ’s efficacy against COVID-19 and help us better understand both the drug and the disease. But there is sufficient credible, scientific data to demonstrate that HCQ has therapeutic value against COVID-19, and that the theoretical risk of harm absolutely does not compare to the very real threat of this disease left untreated. The burden of proof has been met. HCQ should be more widely recommended, prescribed and promoted to treat COVID-19 right now.
Related:
Safety of Hydroxychloroquine among Outpatient Clinical Trial Participants for COVID-19