Source: Medical Journal of Bakirkoy
ABSTRACT
Objective:
As healthcare professionals play a role in combating the COVID-19 outbreak, the risk of disease exposure and illness increases. In our study, we aimed to measure the effectiveness of post-contact use in order to protect the healthcare professionals who work very intensively during the outbreak. Method: A total of 208 healthcare workers who applied to Employee Health Unit section between the dates 25 March-25 April 2020 with a history of contact with COVID-19 patients were included in the study. Employees were evaluated in low, moderate and high risk groups according to the Contact Risk Algorithm included in the Evaluation of Healthcare Workers Guidelines with COVID-19 theme. Three-day hydroxychloroquine treatment was initiated to 138 healthcare professionals who were considered as high risk. The treatment regimen was arranged as 2×400 mg on the first day and 2×200 mg on the 2nd and 3rd days. The COVID-19 positivity rates were analyzed according to the contact risk groups
Results:
There was a statistically significant difference between occupational groups according to contact risk groups (p<0.01); the rate of contact risk of nurses in the middle, and the doctors in the high risk groups was found to be significantly higher. When the COVID-19 positivity rates were analyzed according to the contact risk groups, the COVID-19 positivity rates were 9.4% in the high-, 16.3% in the moderate and 14.3% in the low-risk groups. The contact was found to be related to the COVID-19 test, and the positivity rate from contact with the patient was found to be significantly high (p<0.01).
Conclusion:
Recommendations about hydroxychloroquine for postexposure prophylaxis vary. Hydroxychloroquine can be a possible effective agent in postexposure prophylaxis. We think that conducting similar studies on larger samples can provide significant benefits to individuals and public health.
Keywords:
COVID-19, contact, healthcare workers, hydroxychloroquine
Introduction
Initially a new respiratory virus infection was identified in Wuhan city, Hubei, China, after the number of patients with acute severe respiratory infections increased on December 31, 2019. Since then the outbreak has spread rapidly to other states in China and other countries around the world (1). In January 2020, the causative agent was identified as a novel coronavirus (2019-nCoV) that had not been previously detected in humans by the World Health Organization
(WHO).
Thereafter, the name of the 2019-nCoV disease was accepted as COVID-19 and the virus was named as SARS-CoV-2 due to its similarity to the SARS CoV (2). Findings related to fever, cough, dyspnea and bilateral pneumonic infiltration were detected in
cases. Since the COVID-19 epidemic began in the world, as of May 19, 2020, 316,289 deaths were reported.
Currently, there are 4,735,622 confirmed cases in 212 countries and regions (3). As of the same date, total number of 151,615 cases were reported by the Turkish Ministry of Health (4). Coronaviruses are enveloped and single-stranded RNA viruses of the Coronaviridae family and are known as “crown viruses” due to their crown-like protrusions on their outer surfaces (5). Similar to SARSCoV (26), 2019-nCoV uses angiotensin converting enzyme 2 (ACE2) receptor binding motif (RBM) as receptor (6).
The entry of the virus into the host cells occurs after contact with these specific ACE2 receptors either by endocytosis or membrane fusion. The viral genome must be released for the replication of viruses entering the host cell (1,7). The main routes of transmission for the 2019-nCoV infection are by airborne droplets and direct contact (8). The incubation period is usually 3-7 days and can extend up to 14 days (9).
Personal protective measures, proper isolation and early diagnosis are essential to prevent the spread of infection. Hospital-acquired infection poses a risk to both inpatients and hospital staff. In a clinical series presenting 138 adult patients with 2019-nCoV pneumonia, it was emphasized that 41% of patients were suspected to be infected by nosocomial transmission in hospital (10). As healthcare professionals play a role in the treatment of this disease, their risks of exposure to disease increase. At the same time this situation carries the risk of decreasing health manpower in the fight against the COVID19 outbreak.
China had reported 3387 infected healthcare workers in Hubei Province until February 25, 2020, and at least 18 of these healthcare workers died (11). As of 04.30. 2020, according to the statement of the Turkish Ministry of Health, 7428 employees were infected among 1 million 100 thousand health workers. The rate of this number in average cases is reported to be close to 6.5 percent (12). Up to now no specific effective antiviral therapy for COVID-19 has been found.
Although most COVID-19 patients have mild or moderate prognosis, up to 5-10% of these can contract a disease with a severe, potentially life-threatening course. Yet, there is an urgent need for effective drugs and vaccination (13). Chloroquine and hydroxychloroquine are aminoquinolines, which have been used to treat malaria and autoimmune diseases.
Besides their antimalarial effects, these drugs possess immunomodulatory effects allowing their use for the treatment of autoimmune conditions (14). It has been suggested that HCQ treatment for SARS-CoV-2 infection is more effective in the treatment with its higher lung, blood and plasma concentrations, which reach therapeutic levels within a short time. It is recommended to use 400 mg of HCQ sulfate twice a day for a day and then 200 mg twice a day for a further 4 days (1,15).
Schwartz J. et al. suggested strategies such as preexposure or post-exposure prophylaxis to prevent viral transmission, especially for healthcare workers exposed to SARS-CoV-2 (11). Paglitano et al. also indicated in their studies that hydroxychloroquine can be effective in preventing respiratory invasion in healthcare workers exposed to SARS-CoV-2 and also reported that prophylactic administration of hydroxychloroquine may be beneficial in healthcare professionals participating in high-risk procedures such as intubation, endotracheal aspiration, and bronchoscopy in patients with COVID-19 (16).
Indian Ministry of Health also recommended hydroxychloroquine at a dose of 2×400 mg on the first day, and then once a week prophylaxis for suspected or verified asymptomatic healthcare workers who treated patients with COVID-19 (17). The Health Care Assessment Guideline, whose theme is COVID-19, organized by the Science Board of the Turkish Ministry of Health, also proposed prophylaxis to healthcare workers who came into contact with the COVID-19 patient.
In this guideline, healthcare professionals who come into contact with COVID-19 patients are categorised according to the actions they take during contact (18). In our study, we evaluated the early results of the 3-day prophylactic treatment with hydroxychloroquine which was used for those who were considered high-risk contacts by evaluating the healthcare workers who applied to the Occupational Health and Safety unit of our hospital with a history of COVID-19 contact.
MATERIAL and METHOD:
A total of 208 health workers (doctors, nurses, technicians, pharmacists, clinical secretaries and cleaning staff) who applied to Occupational Health Unit between 25 March – 25 April 2020, were included in the study after being classified according to their ages, genders, professions, work units, additional diseases and smoking statuses.
Healthcare workers in contact with a patient diagnosed with Covid-19, aged 18 and older, with negative serology and PCR (-) at day 0, females with negative pregnancy test who signed the informed consent forms were included in the study. Employees were evaluated in low, moderate and high risk groups according to the contact risk algorithm included in the Health Care Assessment Guideline with COVID19 contact (18).
According to guide, the working group is risk-free if the healthcare personnel use the medical mask all their personal protective equipment appropriately; low risk if not using gloves, gown and glasses;moderate risk if the personnel wears a medical mask with goggles and N95 indication; the risk was considered to be high if they did not use any masks. The risk was considered to be high if they did not use any masks.
Healthcare workers in contact with a patient diagnosed with Covid-19 without a medical mask were considered to be at high risk if they did not use any medical masks or N95. Employees classified as risk-free were not included in the study by explaining the precautions they should take. According to the Ministry of Health COVID-19 theme Health Assessment Guideline (19) the laboratory algorithm was applied depending on the contact health worker risk categories was followed.
Symptoms were monitored for 14 days for healthcare workers included in the low risk class, and active symptom monitoring was performed for those with medium risk; If symptom developed, he was directed to PCR test on the day of symptom, if not on the 7th day. In addition to the follow-up of symptoms, 3-day hydroxychloroquine treatment was initiated for 138 healthcare workers who were considered to be at high-risk.
The treatment was arranged as 2×400 mg on the first day and 2×200 mg on the 2nd and 3rd days. PCR results of the healthcare workers evaluated according to the contact risk were followed on the 7th day; the efficacy of prophylaxis was observed in people who received hydroxychloroquine treatment by classifying the information obtained from PCR (+), and PCR (-) cases.
Statistical Analysis NCSS (Number Cruncher Statistical System) 2007 Statistical Software (Utah, USA) program was used for statistical analysis. While evaluating the study data, Shapiro- Wilk test and box plot charts were used for descriptive statistical methods (mean, standard deviation, median, frequency, ratio) as well as for the normal distribution of variables. One-way Anova test was used in comparing the groups with normally distributed variables, Bonferroni test was employed in determining the group that caused the difference; and Student t test was used in the evaluation of the two groups. In comparison of qualitative data, Pearson Chi-Square test, Fisher’s Exact test and Fisher-Freeman Halton test were used. Significance was evaluated at the level of p<0.05.
RESULTS
The study was conducted on a total of 208 healthcare workers at Bakirkoy Sadi Konuk Research and Training Hospital between March, 25 2020 and April, 25 2020. The ages of the employees varied between 20 and 64, and the average age was 35.18±9.49 years. While,28.4% of the employees were men and 71.6% were women. Examination of the employees distribution based on contact status revealed that 10.1% (n=21) were in the low- risk; 23.6% (n=49) in the moderate and 66.3% (n=138) in the high -risk groups.
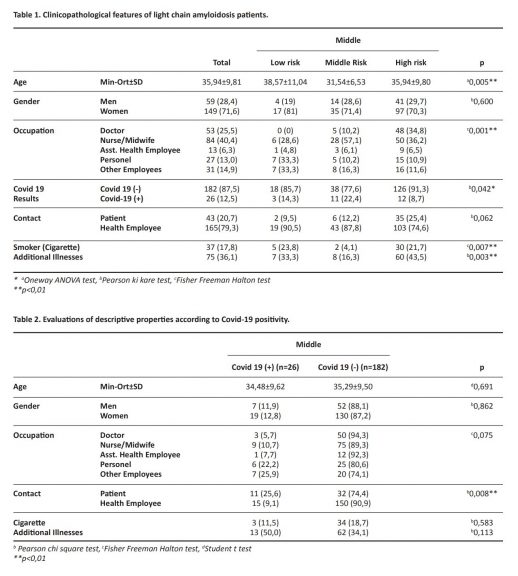
There was a statistically significant difference between the ages by contact risk groups (p<0.01). The average age of the moderate risk group was significantly lower than the low, and high risk groups, respectively p=0.013; p=0.015; p<0.05). There was no significant difference between the average age of low and high risk groups.
There was a statistically significant difference between occupational groups according to contact risk groups (p<0.01). Significantly higher number of nurses were found in the moderate risk group, while doctors were significantly more numerous in the high risk group. Greater number of staff and other employees were also found in the low risk group.
There was a significant difference between COVID19 positivity rates according to contact risk groups (p<0.05). While the COVID-19 positivity rate was 8.7% in the high risk group, this rate was 22.4% in the moderate risk group and 14.3% in the low risk group (Table 1).
According to COVID-19 test results, no statistically significant difference was found between age and gender distributions (p>0.05) No statistically significant difference was found between COVID-19 test results among the vocational groups of health personnel (p>0.05) (Table 2). Contact risk was found to be related to the COVID-19 test –positivity rates , and the positivity rate from contact with the patient was found to be significantly high (p <0.01) (Figure 1).

DISCUSSION
During the epidemic, healthcare workers are concerned about the health of both themselves and their families. Healthcare workers who are accidentally infected are an important source of infection because they can transmit the virus to their families and patients receiving medical care for different reasons, and to other healthcare professionals they work with. As one of the first pandemic hospitals with high patient admission in Turkey, supply of personal protective equipment and necessary training for this equipment were provided from the first day.
According to the Guidelines for Assessment of Healthcare Professionals with the COVID-19 theme organized by the Ministry of Health Science Board of our country, when the hydroxychloroquine prophylaxis was applied to the group with high risk after contact with COVID-19 patients, the COVID-19 test positivity rate was lower in the group which received prophylaxis than the group that did not. COVID-19 test positivity rate was statistically and significantly lower than those in the low and moderate risk groups (p<0.05). However, we could not say that this completely depends on the application of prophylaxis, since we did not have a control group. Twenty-six cases of our healthcare professionals were COVID-19 test positive and their ages varied between 20 and 64, and their mean age was 34.48±9.62 years.
Seven of healthcare workers with COVID-19 test positivity were men and 19 of them were women. Similarly, the risk factors of 72 healthcare workers who had COVID-19 disease in the tertiary hospital in Wuhan, where the COVID-19 epidemic started, were analyzed and 39 health workers were reported to be working in general departments, and their ages ranged between 21-66 years (20). Contact is one of the main transmission ways of SARS-CoV-2. Contagion from patients to healthcare workers is generally the result of contamination of the hands of healthcare workers after touching the patients, and hand hygiene is considered as the most important prevention measure that healthcare workers can take.
When the contact history was examined, the positivity rates from the contact with COVID-19 patients were found to be significantly higher (p<0.01). The results emphasize the importance of hand hygiene after contact with COVID-19 patients, similar to other studies (20,21). According to the contact stories, no significant difference was found between the average ages of the low and high risk groups. It was observed that the highest age average was in the low-risk group and the lowest age average was in the moderate -risk group.
The reason for this may be that the senior healthcare professionals might have used the prevention methods more properly as a consequence of their experience. When the occupational groups were examined according to the contact risk groups; the number of nurses in the moderate and of the doctors in the high risk group was found to be significantly higher. Depending on the intensive working conditions of the healthcare workers during the epidemic,these higher rates may be associated with greater contact load.
Similar to our study in a prospective, observational cohort study in the UK and the USA frontline healthcare workers were found to be at higher risk of reporting COVID-19 test positivity (19). There are different opinions about the application of hydroxychloroquine prophylaxis in healthcare professionals and its protocols. In a post-exposure prophylaxis and preoperative treatment study for COVID -19 conducted by Lother et al. hydroxychloroquine prophylaxis was planned to be applied to asymptomatic healthcare workers or household contacts exposed to COVID -19 cases within four days so as to prevent serious complications of the disease.
Hydroxychloroquine was administered in 200 mg tablets for a total dose of 3.800 mg for 5 consecutive days. Results of the study are expected (22). Some evidence is known about the effectiveness of hydroxychloroquine against this virus and some clinical data to support the effectiveness of this drug in the prophylaxis of infection. However, controlled clinical studies on this subject are ongoing. In our study the rates of nurses and doctors in risk groups were found to be significantly higher. The contact was found to be related to the COVID -19 test, and the positivity rate from contact with the patient was found to be significantly high.
The COVID-19 pandemic, which affects the whole world, continues, health professionals are also working intensively in this process. As contact with patients increases, healthcare professionals’ COVID-19 test positivity rates will also increase. We think that conducting similar studies on larger samples to protect healthcare workers can provide significant benefits to individuals and public health.
Limitations of our study can be stated as follows: 1) long-term results of our study are not yet available 2) follow-up of the participants still continues, 3) lack of a control group in the high-risk group that did not receive prophylaxis. In the guideline published by the Turkish Ministry of Health, prophylaxis is recommended for health workers with high-risk contact history. Therefore, there is no control group in the high-risk group who did not receive prophylaxis. The low number of samples can also be considered as a limitation.
Ethics Committee Approval: For our study, the approval number 2020/144 was obtained from the ethics committee of University of Health Sciences, Bakırköy Dr. Sadi Konuk Training and Research
Hospital.
Funding: None
Conflict of interest: The authors declare that they have no conflict of interest.
Informed Consent: All subjects provided informed consent to participate in the study.
Related:
Vitamin D3 mixed with hydroxychloroquine shows promise in treating COVID-19: Study

